Models of pregnancy care
In some ways, it has never been a more difficult time to navigate pregnancy and birth.
There are books, support groups, classes, and huge amounts of information regarding pregnancy which can be easily downloaded from the internet. However, this abundance of resources means there is simply too much information to process, and too many dissenting opinions out there for the average person to assess and process.
How to manage one’s health during pregnancy
How does a pregnant person get it right? What is the ‘best’ approach for any individual? As you may expect, there is no easy answer to that question. Broadly, pregnancy and birth care can be divided into three schools of thought.
The medical model of care

The first is the medical model of care. This is where pregnancy care is doctor-led, often facilitated by expert care from nurse midwives, and is aimed at prevention or treatment of pregnancy complications. Medical-model care can be aimed at either the public or private system. In the private system, pregnant people will have their own doctor, and be seen in professional rooms, rather than in hospital clinics.
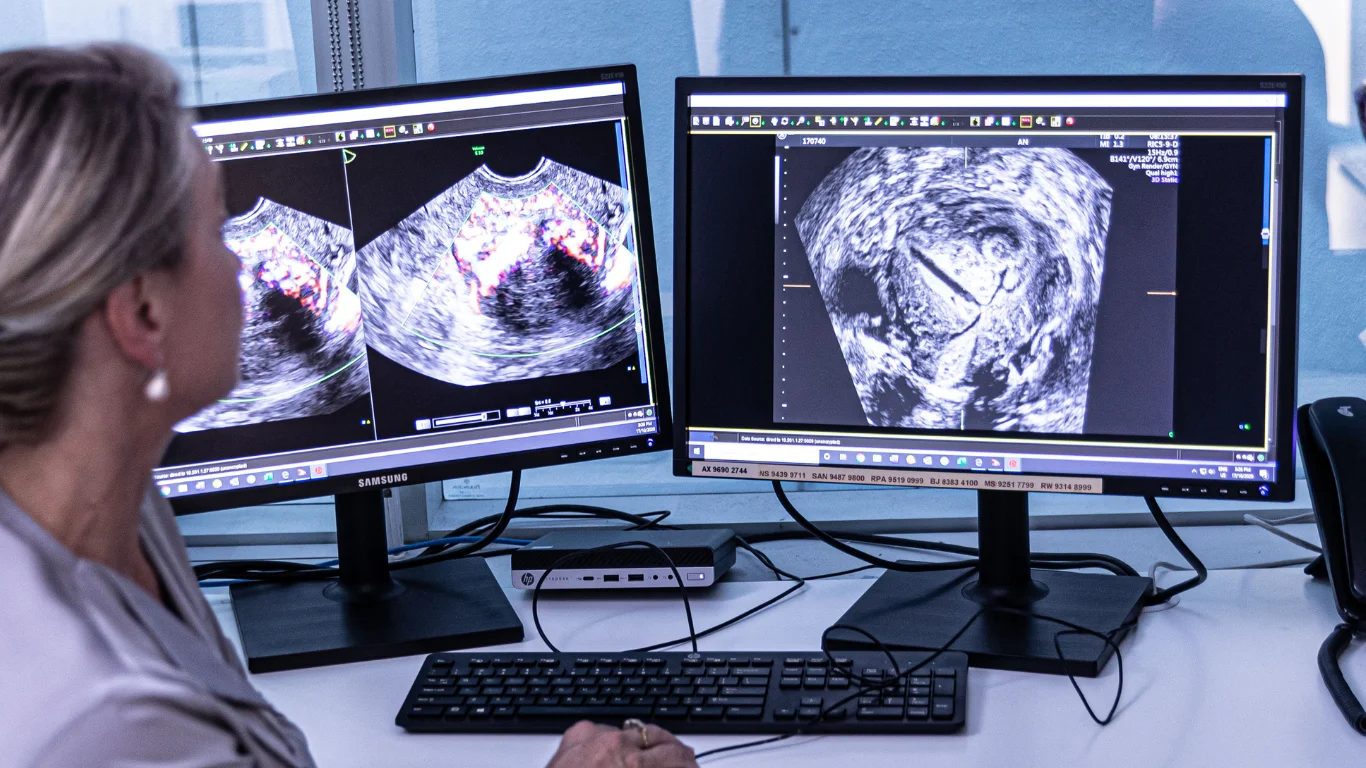
The pregnancy will generally be cared for by a single obstetrician, or a small obstetric group. Some OB’s also employ midwives, for the routine, straightforward portion of obstetric care. Independent prenatal ultrasound practices, such as Ultrasound Care, will provide prenatal diagnostic and pregnancy management services to the individual doctors and patients.
Individualised management
This model of care provides individualised management, including the care during labour and delivery. It’s great to know your own doctor who will be caring for you and also delivering your baby, but that care generally comes with a price – the majority of private care is not covered by Medicare in general, so gap fees will apply.
The good thing about private care in this manner, is that it is easy to research and book with an OB who will have similar thoughts and preferences to yourself regarding your expectations of pregnancy and delivery. It can also be very useful for those who have suffered significant birth trauma in a previous delivery, as knowing that the OB who provides your birth care is aware of your history can be very reassuring.
High risk pregnancy or delivery
Medical-led care is also provided by public hospital clinics, for pregnant people who are considered to be at higher risk during either their pregnancy or delivery. These may include people with multiple pregnancies, severe high blood pressure (hypertension), complex IVF pregnancies, or previous poor outcomes. Most hospitals bend over backwards to provide quality of care and maximum autonomy in pregnancy and delivery, but if there are significant risk factors for a poor outcome, choices of care and mode of delivery may be more limited by the need to ensure safety.
Multi-disciplinary management
It is important to note that being at increased risk of poorer outcomes is not the fault of any person or carer- these things sometimes happen- but that most medical care in this context will be aimed at modifying or managing risk, and ensuring that both mother and baby leave the hospital well and healthy. It can be very disappointing to have the feeling that your choices are being restricted, but there are generally sound reasons behind most high-risk care, and it never hurts to ask to have the relevant reasons explained in detail. It can be disconcerting to feel that every visit seems to be attended by a different health care professional, but the overall care of the clinic is generally in the hands of a senior obstetrician, who will keep tabs on everyone’s progress through pregnancy.
 Midwifery-led care
Midwifery-led care
The second model of care is midwifery-led care. This is generally found in the public hospital system, and is limited to women who are considered to be at low risk of pregnancy complications. The midwifery model is very much aimed at normalising pregnancy, and viewing pregnancy and birth as normal physical processes.
The midwifery teams providing care tend to be close-knit and small, and some hospitals will even offer a small-group midwifery practice, where all care both before and after birth is provided by the same small team, and sometimes care within labour is also provided by that team.
Advantages and disadvantages of midwifery-led care
Midwifery-led care has some significant advantages, in that it can be highly personalised and adds greatly to pregnant people’s sense of autonomy and control over pregnancy and birth. The care is also free of charge. There are a few disadvantages, also, of which to be aware. The first is that, as this model is only aimed at low-risk pregnant people, there is no guarantee that any given person who commences their pregnancy within a midwifery team, will end their pregnancy there. It is also important to note that labour and delivery can be very unpredictable, especially in the first pregnancy, and again there is no guarantee that an easy, complication-free labour and delivery will occur simply because a pregnancy is low risk.
In particular, the amount of discomfort that can be expected during labour and delivery is highly variable, and also cannot be predicted in advance. It is possible to go into labour with the most positive outlook possible, and to still end up with a complicated delivery.
Having realistic expectations
Managing pregnancy effectively is often about managing realistic expectations! The rate of interventions in labour and delivery is lowest in those who attend midwifery clinics, although that may be partially explained by the low-risk nature of the pregnancy population. Not all of the lower intervention rate can be explained by this, as individualised care also leads to a greater chance of a straightforward labour and delivery.
Homebirth midwifery-led care
The final model of care is that of homebirth midwifery-led or even solo (freebirth) birth. This is the ultimate low-intervention model of care in that pregnancy and labour care are all performed at home. Sometimes women do not even have prenatal investigations or ultrasounds. The theory behind in home care is that birth is a natural process, and too often intervened-in by medical professionals.
First “do no harm”
This reasoning ignores the fact that the majority of doctors are also parents, and all health professionals who swear to ‘do no harm’ as part of the most basic conditions of practice.
Nonetheless, homebirth certainly has its adherents, and in parts of Europe, such as Scandinavian countries, is the norm.
A world of difference
There are a few significant differences between Australia and Scandinavia
The first: is that the population may potentially be at lower risk, due to younger age and taller heights (which lower the rates of obstructed labour).
The second: is that the system is highly geared to urgent transfer to hospital if required, and cities are easier to navigate quickly.
Finally: the midwives providing homebirth do not see labour care as an adversarial process, but rather a collaborative process with the hospital and its staff. This can be absent in the Australian community.
Who is suited to homebirth care and what are the advantages and disadvantages
Homebirth care is best suited to pregnant people who are at exceptionally low risk of complications and understand that there is a chance of transfer to hospital, and that the decision may be urgent and need to be performed rapidly. There is also a small chance of very significant complications that may have been managed, in retrospect, in hospital, with better outcomes. For that reason, many doctors do not routinely advocate homebirth, although the enormous majority of homebirths occur safely. If a straightforward labour and delivery are achieved, homebirth can be intensely fulfilling.
 What is freebirth?
What is freebirth?
Freebirth has little or no support from health professionals. This is birth, unattended, at home. The rate of perinatal death of the newborn, is generally considered unacceptable. If a multiple pregnancy or a malposition (breech delivery, for example) occur, the life of both mother and baby will be at significant risk, and rapid transfer to hospital may not achieve a good outcome. Should birth be desired at home, we would always recommend a qualified midwife be present during both the labour and delivery.
Choosing a model that is right for you
There are a number of different models of care that can be considered by pregnant people, partially informed also by that person’s general state of health, the well-being of the fetus, and other factors. There is room in the birthing community for a diversity of opinion, and some models of care will be more suitable than others for any given individual.




 Midwifery-led care
Midwifery-led care What is freebirth?
What is freebirth?